What is Medical Trauma?
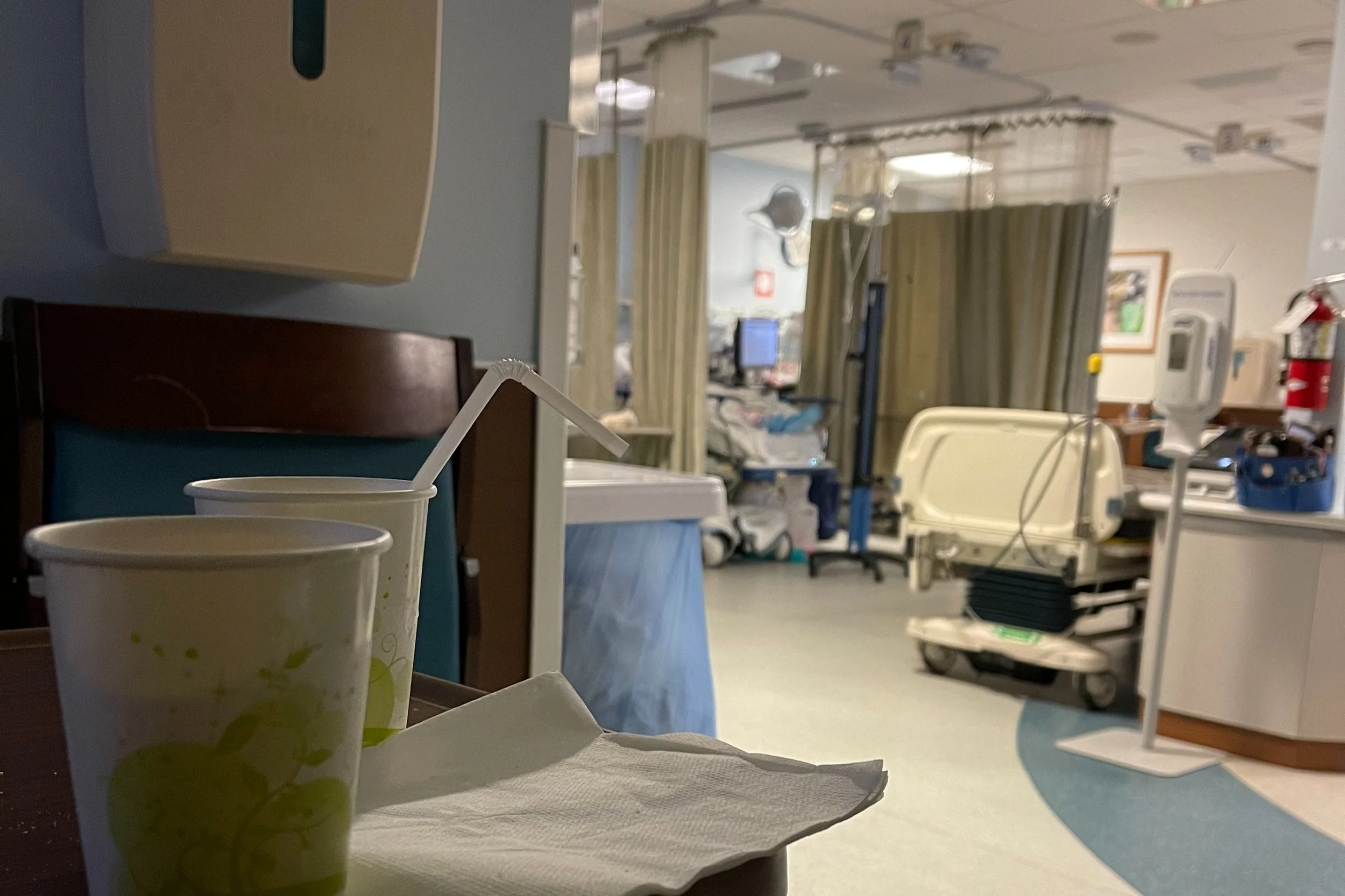
Does this sound familiar?You suffer from a complex illness, chronic pain or one of the many invisible conditions from which 50 million Americans suffer. You walk into your doctor's office anxious, with a long list of medical issues. The doctor seems to be in a hurry and spends a lot of time reviewing your medications and symptoms. Sometimes the PA does this and the doctor walks in without any previous glance at your chart. The doctor may be typing notes on the computer, without eye contact, or any contact for that matter. He or she may ask a few cursory questions, prescribe a medication, and move on to the next patient.
This is the experience of millions of Americans right now. Patients express feeling unheard, uncared for, and dismissed. This is especially problematic for patients with chronic illness, who experience this for years, if not decades. Though it may not feel this way, It's not that doctors don't care; they often care too much, but they only have so much time and so much energy themselves. They still don't know what to do with these complicated cases. They have burnout.
Another common experience is when a patient may feel seen as a medication chart rather than as a person as the doctor asks questions. Again, patients can feel unheard, uncared for, dismissed., and at times afraid. This is especially problematic for patients with chronic illness, for whom a diagnosis is not guaranteed, nor a cure. This is a serious problem and it needs thoughtful action by medical schools to learn about trauma in such a way as to at least understand some of what this patient is going through.
As a trauma therapist and chronic pain patient, I have seen firsthand the devastating impact of medical trauma on patients' health outcomes and on providers' well-being. Medical trauma is defined as a set of psychological and physiological responses to pain, injury, serious illness, medical procedures, and frightening treatment experiences. Although not a formal DSM-V diagnosis, medical trauma is increasingly recognized as a way to understand the additional trauma that patients experience. The result is a silent epidemic that affects millions of people, with women and young women more and more being disproportionately affected. If you are a woman of color, you have ,no doubt, experienced these feelings.
Adverse Childhood Events (ACE) and their relationship to chronic illness are well-documented. Childhood trauma can lead to a range of physical and mental health problems later in life, including chronic pain and illness. Moreover, medical providers are not immune to trauma, and sometimes a medical provider can get triggered by a patient, or the other way around. This can play out in detrimental ways for both parties, leading to misdiagnosis, confusion, isolation, and frustration.
Most of my patients have had some type of trauma, whether related to ACE or illness-induced PTSD from the chronic illness itself. "Classic" PTSD is related to a past event, while illness-induced PTSD (aka Medicial) is experienced as an ongoing threat to the safety of the body. Sometimes that can present itself as agitation or anger. If the trauma is significant, it can obfuscate meaningful conversations with health providers. Patients are frustrated. Doctors are frustrated. Often, at some point, a physician will disengage, feeling they have nothing else they can do for the patient. Or they view the complications as "emotional" and may simply recommend therapy, leaving the patient confused and wondering if the doctor thinks it's all in their head.
My Medical Trauma
I have had too many medical traumas to talk about, but this particular one felt deeper and different. In December 2020, I was suffering with a kidney stone, for weeks before diagnosis and surgery to help could be scheduled. The stone was just a bit bigger than one that could resolve on so it was “stuck” in my ureter tract.
Unbelievably, I was told by my doctor that “this stone couldn’t possibly be the cause of the extreme pain” I was in (ER visits) because it was not moving.
Like I said this wasn’t new territory, I actually like this doctor, he had treated me well in the past, and showed understanding, (or so I thought) about of inflammation and different levels of tolerance to pain. But in 2020, I was at the mercy of him and Operating Room Scheduling. scheduling during a pandemic.
I waited. I was in pain. i couldn’t work. i couldn’t do anything. .We finally got a date December 28, 2020. This waiting was weeks long. Weeks of pain, worsening to depression and fear and hopelessness - hoping the surgery would work, by this point I believed it really was all in my head. Maybe he’s right? maybe it shouldn’t hurt? Was I crazy?
On the day of surgery, he came by my pre-op bed and said “Okay let’s do this. Even though we don’t know why you are on in pain “ (implying it won’t help). He was dismissing my pain, my knowledge of my own body. again. Making me question myself. To me: “Any questions? “. I asked him to please not put a stent in during this surgery unless absolutely necessary; in the past the pain from them was worse than the stones themselves. So, phew. Okay. Lights out! Here’s to the other side I told myself.
I woke up in so much pain. I was given pain control , but to be discharged with Tylenol by the doctor. For a kidney surgery. I asked the nurse, “what if I were a man right now, would they give me adequate pain relief?” She said that if I was a man I wouldn’t be handling as well as I was! And of course they’d prescribe to a man because they can relate to the pain of a stone in a male penis. Ouch they must think, How awful. But you see, they can’t relate to women with pelvic issues. They are invisible, painful and most of us feel ashamed to speak to such things in these sensitive areas.
Not only that; he did put a stent in because of all the damage which he said was not there (what damage I thought, I was supposedly fine and didn’t need surgery according to him).
When I think about this procedure now, I realize I was violated. Essentially he has said, much like a date raper, “okay FINE, we’ll do this because you want to, but I don’t think we need to because it is not causing you pain. “ and then rams a stent up and leaves me with Tylenol. Tylenol. You asked for this remember. This enrages me on behalf of every woman with abdominal and organ pain. More on that to come.
Post-op; this was a relativity easy recovery from a recent procedure. I’m happy that i woke up!!
.
As a therapist, I combine therapy and act as a sort of "medical translator," helping patients navigate the broken medical system. Trauma therapy in conjunction with this approach doesn't "fix" the injury or illness, but it is helpful in allowing the patient to tolerate these stressful appointments through witness and my own experience, as well as the talented team of physicians and therapists at Pain Trauma Institute.
The importance of training doctors and their staff in trauma-informed care cannot be overstated. It is vital that doctors and their staff be trained in trauma and its effects on them. It is equally important that medical providers take care of their staff, with in-house trainings or nature retreats, such as surf therapy with Groundswell Community Project, a partner with Pain Trauma Institute. By doing so, we can create a truly The importance of training doctors and their staff in trauma-informed care cannot be overstated. It is vital that doctors and their staff be trained in trauma and its effects on them. It is equally important that medical providers take care of their staff, with in-house trainings or nature retreats, such as surf therapy with Groundswell Community Project, a partner with Pain Trauma Institute. By doing so, we can create a truly collaborative, integrated model that takes into account the multiple dimensions of trauma, ultimately leading to better health outcomes for patients and less burnout for providers.
Medical trauma is an invisible epidemic that affects millions of people, particularly women and young women. Trauma-informed care is vital for patients and providers to better navigate the broken medical system and improve health outcomes. By acknowledging and addressing medical trauma, we can help Medical trauma is an invisible epidemic that affects millions of people, particularly women and young women. Trauma-informed care is vital for patients and providers to better navigate the broken medical system and improve health outcomes. By acknowledging and addressing medical trauma, we can help patients feel seen, heard, and cared for, leading to empowered patients who will truly participate in their healthcare plan.
If you are experiencing medical trauma or chronic illness, contact us for support.
We are looking for testimonials of interactions with medical providers so we can develop training courses for Medical Providers on how to interact with chronic illness. Submit at connect@paintraumainstitute.com Your info will be kept private, but if you want to post it on our site, that is also possible!